Based on the provided information and an understanding of factors that drive readmissions, the hospital should first
Correct Answer:
D
Reducing Medicare readmissions is a key focus in population health, as readmissions impact patient outcomes and hospital reimbursement under programs like the Hospital Readmissions Reduction Program (HRRP). Factors driving readmissions often include inadequate discharge planning, lack of follow-up care, social determinants of health (e.g., transportation, support systems), and patient-specific risks (e.g., comorbidities). NAHQ CPHQ study materials emphasize a systematic, data-driven approach to quality improvement, particularly for complex issues like readmissions.
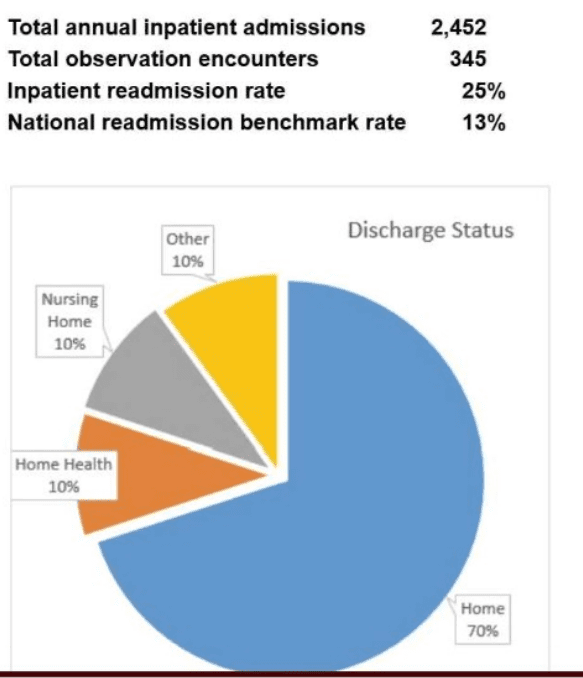
Since the specific Medicare readmission findings are not provided, I'll base the answer on CPHQ best practices. The first step in addressing readmissions should always be to analyze data to determine the best approach for readmission reduction (D). This involves reviewing the readmission findings to identify patterns, such as high-risk patient groups, common diagnoses (e.g., heart failure, pneumonia), or process failures (e.g., medication reconciliation issues). Data analysis helps pinpoint root causes and informs targeted interventions, ensuring resources are used effectively. For example, if data show readmissions are due to lack of follow-up care, then strategies like follow-up calls or visits can be prioritized. Without this analysis, interventions may be misdirected.
Instructing physicians to place patients in observation (A) may reduce reported readmissions by reclassifying stays, but this does not address underlying causes and could be seen as gaming the system, which is not aligned with quality improvement principles. Initiating post-discharge follow-up calls (B) or increasing follow-up visits (C) are potential interventions, but they assume specific causes (e.g., lack of follow-up) without evidence from the data. NAHQ emphasizes that quality improvement starts with understanding the problem through data analysis, making option D the first step.